 |
 |
| 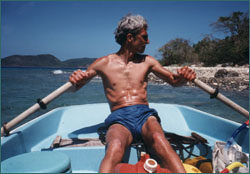 Thomas Holbrook during his
illness
Thomas Holbrook during his
illness
|
One Man's Battle
by Thomas Holbrook
In the spring of 1976, two years into my psychiatric practice, I began
having pain in both knees, which soon severely limited my running. I was
advised by an orthopedist to stop trying to run through the pain. After many
failed attempts to treat the condition with orthotic surgery and physical
therapy, I resigned myself to giving up running. As soon as I made that
decision, the fear of gaining weight and getting fat consumed me. I started
weighing myself every day, and even though I was not gaining weight, I started
feeling fatter. I became increasingly obsessed about my energy balance and
whether I was burning off the calories I consumed. I refined my knowledge of
nutrition and memorized the calories and grams of fat, protein, and
carbohydrates of every food I would possibly eat.
Despite what my intellect
told me, my goal became to rid my body of all fat. I resumed exercising. I
found I could walk good distances, despite some discomfort, if I iced my knees
afterward. I started walking several times a day. I built a small pool in my
basement and swam in place, tethered to the wall. I biked as much as I could
tolerate. The denial of what I only much later came to recognize as anorexia
involved overuse injuries as I sought medical help for tendonitis, muscle and
joint pain, and entrapment neuropathies. I was never told that I was exercising
too much, but I am sure that had I been told, I would not have listened.
Worst nightmare
Despite my efforts, my worst nightmare was happening. I felt and saw myself as fatter
than ever before, even though I had started to lose weight. Whatever I had
learned about nutrition in medical school or read in books, I perverted to my
purpose. I obsessed about protein and fat. I increased the number of egg whites
that I ate a day to 12. If any yolk leaked into my concoction of egg whites,
Carnation Instant Breakfast, and skim milk, I threw the entire thing
out.
 As I became more restrictive, caffeine became more and more important and
functional for me. It staved off my appetite, although I didn't let myself
think about it that way. Coffee and soda perked me up emotionally and focused
my thinking. I really do not believe that I could have continued to function at
work without caffeine.
As I became more restrictive, caffeine became more and more important and
functional for me. It staved off my appetite, although I didn't let myself
think about it that way. Coffee and soda perked me up emotionally and focused
my thinking. I really do not believe that I could have continued to function at
work without caffeine.
I relied equally on my walking (up to six hours a day) and restrictive eating
to fight fat, but it seemed I could never walk far enough or eat little enough.
The scale was now the final analysis of everything about me. I weighed myself
before and after every meal and walk. An increase in weight meant I had not
tried hard enough and needed to walk farther or on steeper hills, and eat less.
If I lost weight, I was encouraged and all the more determined to eat less and
exercise more. However, my goal was not to be thinner, just not fat. I still
wanted to be "big and strong"—just not fat.
Besides the scale, I measured myself constantly by assessing how my clothes fit
and felt on my body. I compared myself to other people, using this information
to "keep me on track." As I had when I compared myself to others in terms of
intelligence, talent, humor, and personality, I fell short in all categories.
All of those feelings were channeled into the final "fat equation."
During the last few years of my illness, my eating became more extreme. My
meals were extremely ritualistic, and by the time I was ready for dinner, I had
not eaten all day and had exercised five or six hours. My suppers became a
relative binge. I still thought of them as "salads," which satisfied my
anorexic mind. They evolved from just a few different types of lettuce and some
raw vegetables and lemon juice for dressing to rather elaborate concoctions. I
must have been at least partly aware that my muscles were wasting away because
I made a point of adding protein, usually in the form of tuna fish. I added
other foods from time to time in a calculated and compulsive way. Whatever I
added, I had to continue with, and usually in increasing amounts. A typical
binge might consist of a head of iceberg lettuce, a full head of raw cabbage, a
defrosted package of frozen spinach, a can of tuna, garbanzo beans, croutons,
sunflower seeds, artificial bacon bits, a can of pineapple, lemon juice, and
vinegar, all in a foot-and-a-half-wide bowl. In my phase of eating carrots, I
would eat about a pound of raw carrots while I was preparing the salad. The raw
cabbage was my laxative. I counted on that control over my bowels for added
reassurance that the food was not staying in my body long enough to make me
fat.
 The final part of my ritual was a glass of cream sherry. Although I obsessed
all day about my binge, I came to depend on the relaxing effect of the sherry.
My long-standing insomnia worsened as my eating became more disordered, and I
became dependent on the soporific effect of alcohol. When I was not in too much
physical discomfort from the binge, the food and alcohol would put me to sleep,
but only for about four hours or so. I awoke at 2:30 or 3:00 a.m. and started
my walks. It was always in the back of my mind that I would not be accruing fat
if I wasn't sleeping. And, of course, moving was always better than not.
Fatigue also helped me modify the constant anxiety I felt. Over-the-counter
cold medications, muscle relaxants, and Valium also gave me relief from my
anxiety. The combined effect of medication with low blood sugar was relative
euphoria.
The final part of my ritual was a glass of cream sherry. Although I obsessed
all day about my binge, I came to depend on the relaxing effect of the sherry.
My long-standing insomnia worsened as my eating became more disordered, and I
became dependent on the soporific effect of alcohol. When I was not in too much
physical discomfort from the binge, the food and alcohol would put me to sleep,
but only for about four hours or so. I awoke at 2:30 or 3:00 a.m. and started
my walks. It was always in the back of my mind that I would not be accruing fat
if I wasn't sleeping. And, of course, moving was always better than not.
Fatigue also helped me modify the constant anxiety I felt. Over-the-counter
cold medications, muscle relaxants, and Valium also gave me relief from my
anxiety. The combined effect of medication with low blood sugar was relative
euphoria.
Oblivious to illness
While I was living this crazy life, I was carrying on my psychiatric practice, much
of which consisted of treating eating-disordered patients—anorexic, bulimic,
and obese. It is incredible to me now that I could be working with anorexic
patients who were not any sicker than I was, even helathier in some ways, and
yet remain completely oblivious to my own illness. There were only extremely
brief flashes of insight. If I happened to see myself in a mirrored window
reflection, I would be horrified at how emaciated I appeared. Turning away, the
insight was gone. I was well aware of my usual self-doubts and insecurities,
but that was normal for me. Unfortunately, the increasing spaciness that I was
experiencing with weight loss and minimal nutrition was also becoming "normal"
for me. In fact, when I was at my spaciest, I felt the best, because it meant
that I was not getting fat.
Only occasionally would a patient comment on my appearance. I would blush, feel
hot, and sweat with shame but not recognize cognitively what he or she was
saying. More surprising to me, in retrospect, was never having been confronted
about my eating or weight loss by the professionals with whom I worked all
during this time. I remember a physician administrator of the hospital kidding
me occasionally about eating so little, but I was never seriously questioned
about my eating, weight loss, or exercise. They all must have seen me out
walking for an hour or two every day regardless of the weather. I even had a
down-filled body suit that I would put over my work clothes, allowing me to
walk no matter how low the temperature. My work must have suffered during these
years, but I did not notice or hear about it.
 People outside of work seemed relatively oblivious as well. Family registered
concern about my overall health and the various physical problems I was having
but were apparently completely unaware of the connection with my eating and
weight loss, poor nutrition, and excessive exercise. I was never exactly
gregarious, but my social isolation became extreme in my illness. I declined
social invitations as much as I could. This included family gatherings. If I
accepted an invitation that would include a meal, I would either not eat or
bring my own food. During those years, I was virtually friendless.
People outside of work seemed relatively oblivious as well. Family registered
concern about my overall health and the various physical problems I was having
but were apparently completely unaware of the connection with my eating and
weight loss, poor nutrition, and excessive exercise. I was never exactly
gregarious, but my social isolation became extreme in my illness. I declined
social invitations as much as I could. This included family gatherings. If I
accepted an invitation that would include a meal, I would either not eat or
bring my own food. During those years, I was virtually friendless.
I still find it hard to believe that I was so blind to the illness, especially
as a physician aware of the symptoms of anorexia nervosa. I could see my weight
dropping but could only believe it was good, despite conflicting thoughts about
it. Even when I started feeling weak and tired, I did not understand. As I
experienced the progressive physical sequelae of my weight loss, the picture
only grew murkier. My bowels stopped functioning normally, and I developed
severe abdominal cramping and diarrhea. In addition to the cabbage, I was
sucking on packs of sugarless candies, sweetened with Sorbitol to diminish
hunger and for its laxative effect. At my worst, I was spending up to a couple
of hours a day in the bathroom. In the winter I had severe Raynaud's
Phenomenon, during which all the digits on my hands and feet would become white
and excruciatingly painful. I was dizzy and lightheaded. Severe back spasms
occurred occasionally, resulting in a number of ER visits by ambulance. I was
asked no questions and no diagnosis was made despite my physical appearance and
low vital signs.
 Around this time I was recording my pulse down into the 30s. I remember
thinking that this was good because it meant that I was "in shape." My skin was
paper thin. I became increasingly tired during the day and would find myself
almost dozing off while in sessions with patients. I was short of breath at
times and would feel my heart pound. One night I was shocked to discover that I
had pitting edema of both legs up to my knees. Also around that time, I fell
while ice skating and bruised my knee. The swelling was enough to tip the
cardiac balance, and I passed out. More trips to the ER and several admissions
to the hospital for assessment and stabilization still resulted in no
diagnosis. Was it because I was a man?
Around this time I was recording my pulse down into the 30s. I remember
thinking that this was good because it meant that I was "in shape." My skin was
paper thin. I became increasingly tired during the day and would find myself
almost dozing off while in sessions with patients. I was short of breath at
times and would feel my heart pound. One night I was shocked to discover that I
had pitting edema of both legs up to my knees. Also around that time, I fell
while ice skating and bruised my knee. The swelling was enough to tip the
cardiac balance, and I passed out. More trips to the ER and several admissions
to the hospital for assessment and stabilization still resulted in no
diagnosis. Was it because I was a man?
I was finally referred to the Mayo Clinic with the hope of identifying some
explanation for my myriad of symptoms. During the week at Mayo, I saw almost
every kind of specialist and was tested exhaustively. However, I was never
questioned about my eating or exercise habits. They only remarked that I had an
extremely high carotene level and that my skin was certainly orangish (this was
during one of my phases of high carrot consumption). I was told that my
problems were "functional," or, in other words, "in my head," and that they
probably stemmed from my father's suicide 12 years earlier.
Physician, heal thyself
An anorexic woman with whom I had been working for a couple of years finally
reached me when she questioned whether she could trust me. At the end of a
session on a Thursday, she asked for reassurance that I would be back on Monday
and continue to work with her. I replied that, of course, I would be back, "I
don't abandon my patients."
She said, "My head says yes, but my heart says no." After attempting to
reassure her, I did not give it a second thought until Saturday morning, when I
heard her words again.
 I was staring out my kitchen window, and I started experiencing deep feelings
of shame and sadness. For the first time I recognized that I was anorexic, and
I was able to make sense of what had happened to me over the last 10 years. I
could identify all the symptoms of anorexia that I knew so well in my patients.
While this was a relief, it was also very frightening. I felt alone and
terrified of what I knew I had to do—let other people know that I was
anorexic. I had to eat and stop exercising compulsively. I had no idea if I
could really do it—I had been this way for so long. I could not imagine what
recovery would be like or how I could possibly be okay without my eating
disorder.
I was staring out my kitchen window, and I started experiencing deep feelings
of shame and sadness. For the first time I recognized that I was anorexic, and
I was able to make sense of what had happened to me over the last 10 years. I
could identify all the symptoms of anorexia that I knew so well in my patients.
While this was a relief, it was also very frightening. I felt alone and
terrified of what I knew I had to do—let other people know that I was
anorexic. I had to eat and stop exercising compulsively. I had no idea if I
could really do it—I had been this way for so long. I could not imagine what
recovery would be like or how I could possibly be okay without my eating
disorder.
I was afraid of the responses that I would get. I was doing individual and
group therapy with mostly eating-disordered patients in two inpatient programs,
one for young adults (ages 12 to 22) and the other for older adults. For some
reason, I was more anxious about the younger group. My fears proved unfounded.
When I told them that I was anorexic, they were as accepting and supportive of
me and my illness as they were of one another. There was more of a mixed
response from hospital staff. One of my colleagues heard about it and suggested
that my restrictive eating was merely a "bad habit" and that I could not
really be anorexic. Some of my coworkers were immediately supportive;
others seemed to prefer not to talk about it.
That Saturday I knew what I was facing. I had a fairly good idea of what I
would have to change. I had no idea how slow the process would be or how long
it would take. With the dropping of my denial, recovery became a possibility
and gave me some direction and purpose outside of the structure of my eating
disorder.
The eating was slow to normalize. It helped to start thinking of eating three
meals a day. My body needed more than I could eat in three meals, but it took
me a long time to be comfortable eating snacks. Grain, protein, and fruit were
the easiest food groups to eat consistently. Fat and dairy groups took much
longer to include. Supper continued to be my easiest meal and breakfast came
easier than lunch. It helped to eat meals out. I was never really safe just
cooking for myself. I started eating breakfast and lunch at the hospital where
I worked and eating suppers out.
 During my marital separation and for a few years after the divorce from my
first wife, my children spent weekdays with their mother and weekends with me.
Eating was easier when I was taking care of them because I simply had to have
food around for them. I met and courted my second wife during this time, and by
the time we were married, my son Ben was in college and my daughter Sarah was
applying to go. My second wife enjoyed cooking and would cook supper for us.
This was the first time since high school that I had had suppers prepared for
me.
During my marital separation and for a few years after the divorce from my
first wife, my children spent weekdays with their mother and weekends with me.
Eating was easier when I was taking care of them because I simply had to have
food around for them. I met and courted my second wife during this time, and by
the time we were married, my son Ben was in college and my daughter Sarah was
applying to go. My second wife enjoyed cooking and would cook supper for us.
This was the first time since high school that I had had suppers prepared for
me.
After ten years in recovery, my eating now seems second nature to me. Although
I still have occasional days of feeling fat and still have a tendency to choose
foods lower in fat and calories, eating is relatively easy because I go ahead
and eat what I need. During more difficult times I still think of it in terms
of what I need to eat, and I will even carry on a brief inner dialogue
about it.
My second wife and I divorced awhile back, but it is still hard to shop for
food and cook by myself. Eating out is safe for me now, however. I will
sometimes order the special, or the same selection that someone else is
ordering as a way of staying safe and letting go of my control over the food.
Toning down
While I worked on my eating, I struggled to stop exercising compulsively. This proved
much harder to normalize than the eating. Because I was eating more, I had a
stronger drive to exercise to cancel calories. But the drive to exercise seemed
also to have deeper roots. It was relatively easy to see how including several
fats at a meal was something I needed to do to recover from this illness. But
it was harder to reason in the same way for exercise. Experts talk about
separating it from the illness and somehow preserving it for the obvious
benefits of health and employment. Even this is tricky. I enjoy exercise even
when I am obviously doing it excessively.
 Over the years I have sought the counsel of a physical therapist to help me set
limits to my exercise. I can now go a day without exercising. I no longer
measure myself by how far or how fast I bike or swim. Exercise is no longer
connected with food. I do not have to swim an extra lap because I ate a
cheeseburger. I have an awareness now of fatigue, and respect for it, but I do
still have to work on setting limits.
Over the years I have sought the counsel of a physical therapist to help me set
limits to my exercise. I can now go a day without exercising. I no longer
measure myself by how far or how fast I bike or swim. Exercise is no longer
connected with food. I do not have to swim an extra lap because I ate a
cheeseburger. I have an awareness now of fatigue, and respect for it, but I do
still have to work on setting limits.
Disengaged from my eating disorder, my insecurities seemed magnified. Before I
had felt as though I was in control of my life through the structure I had
imposed on it. Now I became acutely aware of my low opinion of myself. Without
the eating-disorder behaviors to mask the feelings, I felt all my feelings of
inadequacy and incompetence more intensely. I felt everything more
intensely. I felt exposed. What frightened me the most was the anticipation of
having everybody I knew discover my deepest secret—that there was not
anything of value inside.
Although I knew I wanted recovery, I was at the same time intensely ambivalent
about it. I had no confidence that I would be able to pull it off. For a long
time I doubted everything—even that I had an eating disorder. I feared that
recovery would mean that I would have to act normally. I did not know what
normal was, experientially. I feared others' expectations of me in recovery. If
I got healthy and normal, would this mean I would have to appear and act like a
"real" psychiatrist? Would I have to get social and acquire a large group of
friends and whoop it up at barbecues on Packer Sundays?
Being oneself
One of the most significant insights I've gained in my recovery has been that I
have spent my whole life trying to be somebody I'm not. Just like so many of my
patients, I had the feeling that I was never good enough. In my own estimation,
I was a failure. Any compliments or recognition of achievement did not fit. On
the contrary, I always expected to be "found out"—that others would discover
that I was stupid, and it would be all over. Always starting with the premise
that who I am is not good enough, I have gone to such extremes to improve what
I assumed needed improvement. My eating disorder was one of those extremes. It
blunted my anxieties and gave me a false sense of security through the control
over food, body shape, and weight. My recovery has allowed me to experience
these same anxieties and insecurities without the necessity of escape through
control over food.
 Now these old fears are only some of the emotions that I have, and they
have a different meaning attached to them. The feelings of inadequacy and the
fear of failure are still there, but I understand that they are old and more
reflective of environmental influences as I was growing up than an accurate
measure of my abilities. This understanding has lifted an enormous pressure off
of me. I no longer have to change who I am. In the past it would not have been
acceptable to be content with who I am; only the best would be good enough.
Now, there is room for error. Nothing needs to be perfect. I have a feeling of
ease with people, and that is new to me. I am more confident that I can truly
help people professionally. There is a comfort socially, and an experience of
friendships that was not possible when I thought that others could only see the
"bad" in me.
Now these old fears are only some of the emotions that I have, and they
have a different meaning attached to them. The feelings of inadequacy and the
fear of failure are still there, but I understand that they are old and more
reflective of environmental influences as I was growing up than an accurate
measure of my abilities. This understanding has lifted an enormous pressure off
of me. I no longer have to change who I am. In the past it would not have been
acceptable to be content with who I am; only the best would be good enough.
Now, there is room for error. Nothing needs to be perfect. I have a feeling of
ease with people, and that is new to me. I am more confident that I can truly
help people professionally. There is a comfort socially, and an experience of
friendships that was not possible when I thought that others could only see the
"bad" in me.
I have not had to change in the ways that I initially feared. I have let myself
respect the interests and feelings that I have always had. I can experience my
fears without needing to escape.
 Thomas Holbrook today
Thomas Holbrook today |
|
Thomas Holbrook, M.D., is Clinical Director of the Eating Disorders Program at
Rogers Memorial Hospital in Oconomowoc, Wisconsin. He has been treating men for
20 years in his psychiatric practice. This article was adapted with permission
from Making Weight: Men's Conflicts with Food, Weight, Shape, and
Appearance, by Arnold Andersen, M.D., Leigh Cohn, M.A.T., and Thomas
Holbrook, M.D. (Carlsbad, CA: Gürze Books, 2000). |
Photos: Courtesy of Dr. Thomas Holbrook
Ask the Experts |
Watch the Program |
Share Your Story
Help/Resources |
Minority Women: The Untold Story |
One Man's Battle
Body Needs |
Transcript |
Site Map |
Dying to be Thin Home
Editor's Picks |
Previous Sites |
Join Us/E-mail |
TV/Web Schedule
About NOVA |
Teachers |
Site Map |
Shop |
Jobs |
Search |
To print
PBS Online |
NOVA Online |
WGBH
© | Updated December 2000
|
|
|